A peek into the unconscious brain under anesthesia
In our everyday lives we are aware of ourselves, our behavior, and the sensory perception of our environment. This awareness during awake states is known as consciousness. As much as it is central to our brain activity, it has also been one of the greater mysteries of neuroscience. In our lifetimes we all experience changes in our state of consciousness, particularly in the alternation between sleep and wake states. We may also experience changes in consciousness state when fainting, during an epileptic seizure, and through the effects of psychoactive drugs. What is happening in our brains when our conscious selves are not present?
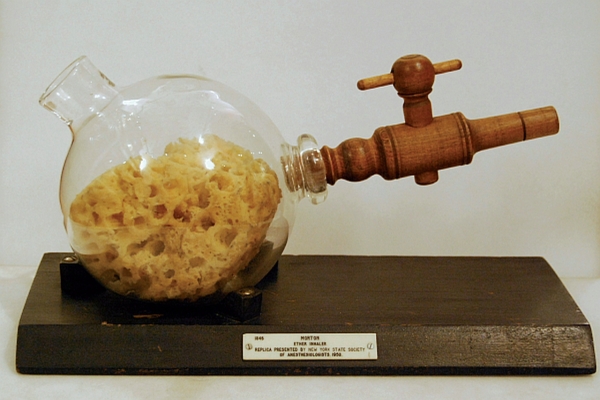
Morton’s ether inhaler, as used in one of the first successful demonstrations of general anaesthesia in October 1846. (6)
For many psychoactive drugs we have little to no idea of how they act on the brain. A small group of these drugs, though very dissimilar in their chemical composition, induces in our brain a state of loss of consciousness, known as anesthesia. The word anesthesia comes from the ancient Greek an (without) and aesthesis (sensation). In this state, however, we don’t simply undergo a loss of sensory perception, we also lose awareness, or consciousness. Medically, general anesthesia is described as a combination of paralysis, analgesia, amnesia and unconsciousness. These qualities have made it a common practice during invasive medical and surgical procedures.
Anesthesia is often referred to as sleep, but this comparison is very misleading. For example, someone undergoing anesthesia cannot be aroused and is unresponsive not only to verbal, but also to noxious stimuli. The differences between these states of unconsciousness were studied using electroencephalograms (EEG). The EEG allows us to non-invasively monitor cortical brain electrical activity patterns, albeit at a low resolution. The EEG records oscillatory patterns of synchronized activity from groups of cortical neurons through the skull and scalp, and these are thought to be representative of the activity of neurons and neural circuits.
The EEG registers patterns of electrical oscillations that are classified based on frequency. Distinct frequency patterns are used as signatures to recognize the state of the brain. For example, in humans, awake and conscious states are characterized by a range of high frequency alpha, beta and gamma oscillations. A much lower frequency is reached for example during non-REM sleep, which is characterized by slow delta waves (see Fig.1)2.

Overview of common EEG patterns and their frequencies.(Purdon et al., 2015)
The signature of a brain under anesthesia is composed of several stages of sedation and unconsciousness, but it is also very different based on the administered anesthetic. The most common anesthetics are of three classes: ether derivatives (such as isofluorane and sevofluorane), GABA receptor binding drugs (such as propofol, barbiturates, benzodiazepines) and NMDA antagonists (such as ketamine). The discrepancy between the different chemical composition of anesthetics, their different affected targets in the brain, and the similarity in the effect on our state of consciousness is a puzzling dilemma in the understanding of anesthesia. The action on GABA receptors (of propofol, for example) leads to a hyperpolarization of postsynaptic neurons in cortex and thalamus; the high interconnectivity between these two regions is thought to be reflected in the recorded electrical signal1. The EEG signature shows a decrease in oscillation frequency, termed alpha and beta oscillations (see Fig.1). Ethers produce a very similar EEG pattern and are therefore also thought to act on GABA receptors.
However, not all anesthetics decrease oscillatory frequency. As an NMDA antagonist, the action of ketamine is distinctly different. At low doses it reduces activity of inhibitory neurons, leading to enhanced activity characterized by euphoria, dissociative states and hallucinations. At higher doses a state of unconsciousness is reached, but the EEG still shows high levels of activity characterized by gamma burst and beta-gamma oscillations (see Fig.1)4. This pattern of activity is apparently in contradiction with the state of unconsciousness. Several explanations have been proposed for this discrepancy. Neuronal hyperactivity also causes loss of consciousness during epileptic seizures, which are characterized by organized bursts of hyperactivity that disrupt the normal function of neural circuits. Some have compared this mechanism to the anesthetic effect of ketamine2. Recent work by Akeju and colleagues (2016), instead, suggests that slow delta oscillations in the gamma-burst phase are the key to understanding this state of unconsciousness. They propose that these slow delta waves result from a reduced activity in the NMDA-mediated arousal pathways emanating from the brainstem4.
EEGs during different states of conscious can also teach us something about the development and aging of our brains. Recent studies have looked into these processes and have shown that the EEG patterns induced by anesthetics differ with age. While elderly patients are more prone to present burst suppression associated with deeper states of unconsciousness5, infants lack many of the characteristic patterns of activity. A study by Cornelissen and colleagues (2015) in infants from 0-6 months after sevofluorane (a highly fluorinated methyl isopropyl ether) administration shows that while they present slow delta-oscillations, theta and alpha oscillations emerge only after 4 months of age. What I thought was most striking was their observation that none of the infants presented frontal alpha wave predominance and coherence3. It had previously been observed in adults that the EEG during anesthesia-induced unconsciousness shows not only a change in thalamocortical oscillation frequency, but is also characterized by spatial coherence of slow alpha oscillations in the frontal cortex. This suggests that during unconsciousness thalamocortical circuits present structured rhythmic activity patterns. These patterns disappear however when a deeper (and more dangerous) state of unconsciousness is reached characterized by burst suppression in the EEG-recorded activity. The observation that infants do not show these structured rhythmic patterns of activity might be related to different degrees of GABAergic innervation of cortical neurons during infancy. It should be noted that the EEG of infants is very different from that of adults, also during awake states when it presents low frequency oscillations. This leaves us to wonder what this can teach us about the differences in the states of consciousness and unconsciousness in infants and adults.
This observation, along with the careful characterizations of cortical oscillations during varying states of consciousness, raises questions as to how these rhythmical activity patterns are generated and how they mediate our awareness, and maybe also sensory perception of the environment. Anesthetic drugs demonstrate an incredible elasticity in the brain’s state of arousal, as it is most often able to readily return to consciousness and arousal as the drugs wear off. Understanding what happens in an unconscious brain, and how it returns to awake states can teach us a great deal about the conscious brain as well, and how it develops through infancy.
Bibliography
- Purdon P.L., Sampson A., Pavone K.J., Brown E.N. (2015) Clinical Electroencephalography for Anesthesiologists: Part I: Background and Basic Signatures, Anesthesiology, 10(123), 937-960.
- Brown E.N., Lydic R., Schiff N.D. (2010) General Anesthesia, Sleep, and Coma, The New England Journal of Medicine, 363(27), 2638-2650.
- Cornelissen L., Kim S., Purdon P.L., Brown E.N., Berde C. B. (2015) Age-dependent electroencephalogram (EEG) patterns during sevoflurane general anesthesia in infants, eLife, 4:e06513.
- Akeju O., Song A.H., Hamilos A.E., Pavone K.J., Flores F.J., Brown E.N., Purdon P.L. (2016) Electroencephalogram signatures of ketamine anesthesia-induced unconsciousness, Clinical Neurophysiology, 127, 2414-2422.
- Brown E.N., Purdon P.L. (2013) The aging brain and anesthesia, Curr Opin Anesthesiol, 26, 414-419.
- Image from: http://oxfordmedicine.com/view/10.1093/med/9780199564217.001.0001/med-9780199564217-chapter-1.
